By Allegra Tepper
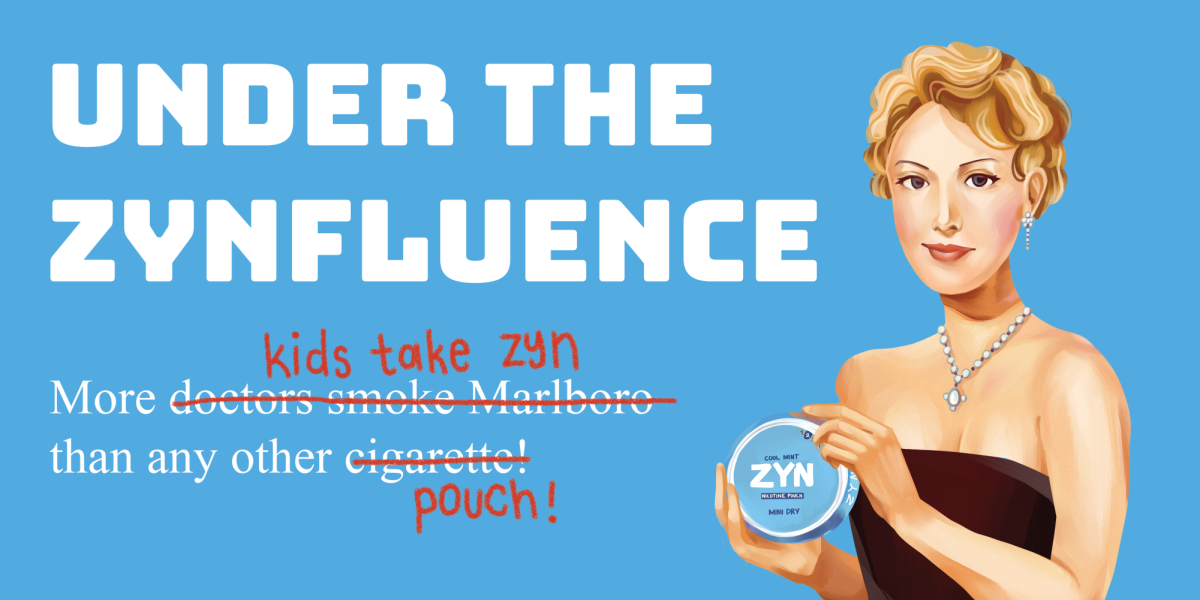
Marcia,* 17, isnât sexually active and doesnât plan to be for a while. Sheâs seen her friends come in to school, bandaged after receiving a Gardasil shot, which has gained notoriety as one of the more painful in the cabinet.
“I see no reason to put myself through that kind of pain if I donât have to,” Marcia said.
As a matter of fact, she can and she should. Gardasil, a vaccine made by Merck & Co., is a shot series that helps protect girls from cervical cancer and genital warts. According to a survey of 75 upper school female students campus, 70 percent of Harvard-Westlake females have received the Gardasil vaccine.
Until recently, that was the only relevant demographic. The Food and Drug Administration will be approving Gardasil for males aged 9 to 26 in the next two weeks, said Robin Farias-Eisner (Gina â03, Anna â05, Joe â06, Anthony â09, Nicolena â13) Chief of Gynecology and Gynecologic Oncology at the University of California, Los Angeles Medical Center.
The vaccine, which includes three shots administered over the course of six months, prevents human papillomavirus, or HPV. According to the Centers for Disease Control, HPV is the most common sexually transmitted disease and approximately 80 percent of adults in the United States have had some form of the virus.
Since its FDA approval for women ages 9-26, Gardasil has been marketed heavily to women with the “One Less” campaign. Alex Glancy â10 believes the campaign has been effective.
“I feel very proud to be a woman when I think about it,” Glancy said. “Itâs like a feminist thing; no guys allowed.”
Well, not anymore. With the new approval, Merck will now need to broaden its target demographic.
“Men are the ones that give it to women,” said Andrea Stein, a gynecologist who administers the vaccine at her Santa Monica practice.
Stein suggested that all male teenagers talk to their pediatrician or internist about the vaccine. Before making the obvious conclusion that the male Y chromosome is impervious to cervical cancer, males should know that the vaccine prevents HPVs 16 and 18, two strains that cause significant percentages of anal and penile cancers.
Studies published by the National Cancer Institute show that efficacy in males is the same as that for females, both at 98 percent, Farias-Eisner said.
In addition to strains 16 and 18, Gardasil prevents strains 6 and 11, which arenât included in any other vaccines of its kind.
HPV has upwards of 130 different strains, and while Gardasil prevents four of the most dangerous, there are still 25 to 30 others that fall into that category.
“It doesnât give you permission to say that I am not going to get HPV by any stretch of the imagination,” Stein said.
Aliana,* now 17, had already been sexually active with her boyfriend for nearly eight months when she arrived at her pediatricianâs office for a physical. She was 15 and having sex on a regular basis, ranging from “tri-weekly to bi-daily.” Upon learning this, Alianaâs pediatrician was adamant that she get the Gardasil vaccine. Thinking that the shots were intended to be administered before one was sexually active, Aliana thought the ship had sailed.
But Stein said that girls like Aliana should absolutely still head in to their pediatrician or gynecologist for the vaccination.
Since both Aliana and her boyfriend were previously virgins and monogamous at the time, neither one was at risk of having HPV or transmitting it to their partner.
However, in the case that an individual is sexually active with multiple partners and has potentially gotten the virus, it is still important to have an examination and get the vaccine, Stein said.
“While around 80 percent of sexually active men and women have had a strain of HPV, itâs unlikely that theyâve had all four that Gardasil prevents,” Stein said. “Your body has built up antibodies once the virus has cleared, but it is important to protect yourself against the other strains.”
Young adults like Marcia who are not sexually active and donât plan to be for a while still ought to consider the vaccine, regardless of the pain, Stein said.
“Someone who is technically a virgin can still get HPV from receiving oral sex,” Stein said. “Itâs a very individualized thing, and there are cases for which it doesnât make sense to get the shots, but for the majority of people, itâs important.”
While the FDA has approved the vaccine only for individuals between the ages of 9 and 26, Stein recommends Gardasil to her patients 26 and older who are sexually active with more than one partner.
“I am also strongly backing the use of the vaccine in females older than 26,” Farias-Eisner said. “The request has been put in for women between the ages of 26 to 45, and that will follow approval for males, within the next 18 months.”
The vaccine is a preventative measure, especially for young women as they get older and are at a higher risk for cancer. HPV that isnât cleared can linger and turn abnormal cell cancerous over time. According to the CDC, cervical cancer is the most common cancerous result of HPV, but the virus can also lead to cancers of the genital region in both sexes.
About 10 percent of infected women will develop long-lasting infections that put them at risk for cervical cancer, according to the CDC. Due to the incidence in developing countries, cervical cancer is the second most common cause of fatality among young women after trauma, Farias-Eisner said. Genital warts are a sign of HPV, and Stein recommended that both males and females use a mirror to periodically check for abnormalities.
Even after receiving the vaccine, Steinâs mantra for her patients remains the same: “Condoms, condoms, condoms.”
“There are still 25 other strains of HPV that are dangerous, and the vaccine does not prevent any other STDs,” Stein said. “This is no substitute for contraception.”
*Names changed upon request